Understanding the 3 Distinct Stages of Adrenal Fatigue
Typically, adrenal fatigue sufferers go through 3 stages, which characterize this syndrome’s progression from perfect health to complete exhaustion. Each stage affects your body differently. Learn to identify the symptoms of adrenal fatigue in different stages of the condition, so you can make the right decisions for recovery.
All too often, patients who suffer from the effects of adrenal fatigue fail to see the warning signs in advance. For many, life continues on as they grow weaker and weaker, and the pattern of deterioration in their health doesn’t capture their attention until it is too late. That’s unfortunate, since many of the worst effects of this syndrome can be averted when patients are aware of what is happening to their bodies.
The good news is that there are three distinct stages of adrenal fatigue, and they can be recognized if you know how to identify them.
In the most general sense, the 3 stages of adrenal fatigue include:
- alarm reaction
- resistance reaction
- burnout and exhaustion
Your ability to recover will vary depending upon which stage you are in when you recognize your symptoms. Obviously, awareness of the problem during that alarm stage can make recovery significantly easier than if you allow the symptoms and signs to continue into the resistance stage. And, as you may already know, once you reach the full burnout stage, recovery from that level of exhaustion can take a year or longer.
We’ll examine each stage independently and note how your body reacts to what is happening to it.
1st Stage of Adrenal Fatigue: Alarm Reaction
The first stage is known as the alarm reaction. This is the stage of the progression toward full exhaustion that is commonly referred to as the “fight or flight” reaction – an instinctual response of the body to any perceived threat. This natural response has been part of the human condition for as long as mankind has existed. Our ancient ancestors may have faced different types of stress, but their bodies responded to each instance of outside pressure in precisely the same way that ours do today.
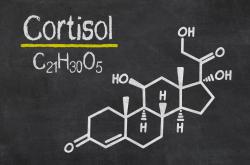
The problem with that instinctive response should be obvious when you consider the different lifestyles we lead today and contrast them with the dangers faced by ancient man. In previous eras, humans faced a wide variety of physical dangers – from the environment, from the beasts of the field, and from other men. When stress is detected by the hypothalamus and the body is flooded with cortisol in an attempt to create the energy needed to either fight or flee, that natural response is ideal for the kind of dangers that were such an inherent part of ancient life. That same natural response is less ideal for today’s most common forms of stress.
Today’s most common stressors are far less likely to involve the type of danger that requires people to actually fight or flee, and far more likely to involve mental and emotional stress, health concerns, and other factors that never actually threaten lives. And yet the body still reacts with that same primal response mechanism, flooding the system with cortisol and other hormones to ensure that the stressed individual has the energy he needs to engage in battle or run away – even when there is nothing to actually fight or run away from!
In a potential battle situation, this response is a life-saver. When you’re frustrated because you’ve been stuck in line waiting to renew your driver’s license, however, that influx of cortisol and other related bodily changes are not helpful at all. In fact, they are downright harmful. Instead of that energy being released in a fight for survival or a mad dash to safety, it ends up being vented in frustration, anger, or some other negative emotion. Or it ends up increasing your level of agitation, as you bottle up your emotions and allow the stress to build. Obviously, our modern lifestyles do not always comport well with our primal stress response.
How the Alarm Works
To understand how this alarm reaction works, it can be helpful to look at the process your body undergoes as it moves from a state of relative calm to a status of high alert and anticipation of danger. It doesn’t really matter what the outside stressor might be either. Regardless of whether you’ve just been fired by your boss or find yourself stressed out by an unexpected bill that needs to be paid, the body responds with one consistent response: it sounds the alarm and marshals its forces in anticipation of what it always assumes will be a full-blown crisis situation.
Here’s what that mobilization looks like, as the body sends forth its hormones, and those chemicals work to make subtle changes to the body to prepare it for whatever danger it may face:
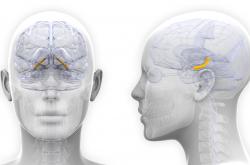
- At the first sign of stress, the hypothalamus springs into action. Responsible for exercising control over the body’s chemical reactions, this small grouping of brain cells has an impact far in excess of what its diminutive size might otherwise suggest. As part of the limbic system, it is in part responsible for many of the body’s most primal instincts – especially those that involve sex and survival.
- Once the hypothalamus is roused, it sends a signal to the pituitary letting it know that danger is imminent. This signal triggers a response from that receiving gland that results in the release of ACTH (adrenocorticotrophic hormone).
- That ACTH travels to the adrenal glands, where it stimulates those glands to begin releasing cortisol, adrenalin, noradrenalin, and the other hormones the body needs for stress management.
- Once these hormones are released, they being to spread out through the body and summon all your physical resources in preparation for whatever physical action you need to take to deal with the perceived threat.
- As your cortisol levels increase during this process, they begin their task of ramping up the conversion process for turning glycogen reserves into the glucose needed to elevate your blood sugar and create energy for the body’s cells.
- Meanwhile, oxygen levels are elevated throughout the brain, heart, and muscles due to respiration changes caused by this hormonal response. The pace of your breathing quickens even as it becomes shallower.
- Blood is siphoned from the intestines for use elsewhere during the crisis.
- As the adrenal medulla releases adrenalin and noradrenalin, its entry into the blood provides a sudden explosion of energy that your body can use for its physical response to the stress.
- Your muscles become tense, your heart rate becomes elevated, and blood vessels become dilated. This leads to an increase in your blood pressure that continues as more adrenalin and cortisol are secreted.
- Perspiration begins as a direct response to the presence of heightened levels of cortisol.
- The rectum and bladder lose tension.
- Digestion slows and then ceases, as the hypothalamus shuts down every system that is not directly related to dealing with the crisis at hand.
As the process continues, your sex hormone and DHEA levels can drop dramatically, as all of the nutrients and other resources needed for producing those hormones are siphoned away for use in the production of cortisol and the other stress hormones. In the early phase of the alarm stage, lab tests would indicate elevated cortisol, insulin, adrenalin, noradrenalin, and DHEA. By the time the body is well into the process of preparing for action, those DHEA levels will have plummeted.
All of that adrenal activity does produce some noticeable signs even during this early part of the progression. Often times, patients report being extremely tired, but vigilant and somewhat energetic at the same time. This often leads to that general state of alertness that many people exhibit throughout the day – a state that is often maintained through the use of coffee and other stimulants, mind you – that is then followed by a dramatic crash in the evening as energy levels drop off precipitously.
You’ve probably heard tales of how a young mother performs a seemingly superhuman feat of strength after an accident – like lifting her car to rescue her trapped baby. It is this cascade of hormones that makes such feats possible during moments of extreme stress! As a general rule, though, this supercharged period of heightened hormonal levels only lasts for minutes or several hours before the body begins to return to normal.
That recovery period can take a day or two, and is characterized by a marked reduction in cortisol production. As a result of the dramatic changes that were needed for that stress response, the body is far less capable of managing new stress during that recovery. In fact, most of the systems involved in that first response will effectively stop responding to new emergency calls during that period. It’s somewhat akin to a fireman responding to a fire alarm, rescuing a family from a burning home, and then going home and taking the phone off the hook so no one else can call him while he is resting.
There’s a problem with this system though, and one that reveals just how unsuitable our primal reactions are when it comes to dealing with modern stress. What do you do when that single emergency never seems to end, or if new stress situations arise in rapid succession after the first episode? When that happens, your body reacts by entering what we call the resistance stage.
2nd Stage of Adrenal Fatigue: Resistance Reaction
The resistance reaction occurs anytime you’ve experienced a powerful stress situation, subsequently recovered, and then been hit with additional stress. Now, that doesn’t mean that you had fully recovered, of course. The effects of the first stressor often continue to linger on throughout the entire progression from full health to exhaustion. What happens is that your body responds to the continued presence of stress by focusing its attention on a continuing high level of stress hormone production.
That, of course, means that less DHEA and sex hormone is produced, as your adrenals continue to choose cortisol production over the less useful sex chemicals. To manage that prioritization, the adrenals divert the hormone pregnenolone away from sex hormone production and devote all of it to manufacturing cortisol. That creates an imbalance that can lead to loss of energy, a lowering of enthusiasm, diminished libido, and greater susceptibility to illness and infection.
From the body’s point of view, this is a necessary tradeoff to ensure that it has the resources it needs to continue its battle against stress. This resistance to the normal cycle of response and recovery has an obvious benefit in that it can enable someone to remain in survival mode even after that first fight or flight reaction is done. That can be extremely useful in real combat situations, or for first responders or disaster aid workers who are faced with days or weeks of stressful battle or rescue operations.
To maintain that level of readiness, cortisol levels must remain elevated so that the hormone can continue its work of converting carbohydrates, protein, and fats into the essential energy the body needs to maintain physical activity. This constant conversion of food to energy is known as gluconeogenesis, and provides the means by which high energy levels can be supported even when the body’s glucose stores have already been used. To ensure that everything remains at optimal levels, that cortisol also works to encourage the body to maintain higher levels of sodium so that the heart remains strong and blood pressure remains at a higher level that is more conducive to action.
Here’s where this begins to spell trouble for your health. As this process continues indefinitely, your adrenals never get a chance to return to normal cortisol levels. That can quickly lead to problems, since the human body is simply not designed to withstand high levels of cortisol for prolonged periods of time. That’s because cortisol’s effects go beyond glucose conversion. This hormone is also an anti-inflammatory that can weaken the immune system when it is present at high levels.
That means that a sustained resistance reaction will result in a heightened chance that the patient will contract an illness or serious disease like cancer or diabetes. This occurs due to the overstimulation of the cells of the body that occurs when cortisol remains at higher than normal levels for too long. To make matter even worse, the resulting weakness and potential illness can place additional stress on the adrenals, making it even more difficult for them to produce cortisol to respond to the pressure, and further weakening the entire system.
During this stage of the progression – a stage that can last for years or even decades, the body will do its utmost to keep pace with the demands placed upon it. Each new stress will result in subtle adaptations as the systems of the body try to make the changes needed to ensure their survival. In the end, though, this stage will inevitably lead to exhaustion if steps are not taken to reverse the situation and provide the adrenals with the relief they need. Without such a reversal, however, the body will continue to weaken until full fatigue sets in.
3rd Stage of Adrenal Fatigue: Burnout and Exhaustion
Once you’ve reached the point of exhaustion, almost anything can happen. Your entire body can simply shut down or you can experience a loss of function in any of its various systems. This is the natural result of a decrease in hormones like aldosterone, as well as the gradual depletion of both the levels of cortisol in the body and the adrenal glands’ ability to produce that hormone. While everything might seem manageable during the resistance stage of the progression, things can deteriorate quickly once the burnout begins to set in.
So what does that exhaustion look like as you enter this third and final stage of adrenal fatigue? Here are just a few of the negative effects that you will experience:
- As a result of that depletion of cortisol and aldosterone, your sodium levels will plummet from the abnormal highs they enjoyed during the resistance stage. At the same time, you’ll experience an increased rate of potassium retention, and a drop in glucose production which can lead to hypoglycemia. This will create an imbalance in critical electrolytes.
- That imbalance will cause the cells to lose their ability to function normally, since they rely on normal levels of glucose and the right balance between those vital minerals.
- Without the right electrolytes and blood sugar levels, your entire body will begin to feel weak.
- As this continues, your ability to create cortisol diminishes, further depriving you of the glucose you need to provide energy for your body. This leads to the cravings for sugar and various stimulants that are so common in adrenal fatigue patients.
- Eventually, your cells become unable to operate as designed, and grow more and more damaged as time goes by. Even when you replenish those nutrients, the cells will use most of that energy just to jumpstart their own activities, leaving little behind for use in physical activity.
- The end result: even food will provide little actual energy once you’ve reached a state of compete exhaustion.
At that point, one of two things can happen. You can either continue in that state until your entire system collapses and your adrenals become completely unable to respond to any stress – which can leave your kidneys damaged from lack of aldosterone, or you can take affirmative steps to reverse the damage.
Every Case is Different
It is important to remember, of course, that every case is slightly different. While there are definable stages through which this syndrome progresses, the pace of that progression can vary from individual to individual. More importantly, each individual adapts to this progression in his or own unique way. Sometimes, a person can enter the exhausted stage after only one stressor and a brief period of resistance. Other people can go for decades in a state of resistance and then collapse into exhaustion. Still others appear to be on a rollercoaster of fatigue and recovery. Finally, there are those whose bodies just seem to steadily lose their ability to respond to stress, with little noticeable resistance.
As a general rule, however, the three stages of adrenal fatigue outlined here are the human body’s common response to high levels of stress, especially stress that is either constant or repetitive in nature. The fact is that our physiology was designed for a time when physical responses to stress were premised upon actual physical danger. As we’ve become more “civilized” and our stress has become less susceptible to physical resolution, it is those physical responses that often pose the greatest danger to us in any stressful situation.
By learning to recognize the various stages of fatigue, your odds of identifying fatigue early in the progression are increased dramatically. That can enable you to make the lifestyle changes you need to ensure that your health is safeguarded from further harm. And that can often provide you with the opportunity you need to avoid compete exhaustion and recover from your adrenal fatigue as quickly as possible.
You might also be interested in:
- Adrenal Syndrome - The 3 Stages of Adrenal Exhaustion. http://www.coreonehealth.com/the-3-stages-of-adrenal-exhaustion
- Adrenal Stress Index: Seven Stages of Fatigue. http://www.livestrong.com/article/206543-adrenal-stress-index-seven-stages-of-fatigue/
- Stage 3 Adrenal Fatigue. http://www.adrenaladvice.com/stage-3-adrenal-fatigue.shtml
- Stage 3 Adrenal Fatigue--(Adrenal Exhaustion). http://www.mdjunction.com/forums/lyme-disease-support-forums/medicine-treatments/2997768-stage-3-adrenal-fatigueadrenal-exhaustion












.jpg)



Leave a comment